Tissues & Organs
DIGESTIVE SYSTEM
General Histology
Esophagus
Stomach
Small Intestine
Duodenum
Jejunum
Ileum
Colon
Appendix
Rectum & Anus
Pancreas
Tissues & Organs
DIGESTIVE SYSTEM
General Histology
Esophagus
Stomach
Small Intestine
Duodenum
Jejunum
Ileum
Colon
Appendix
Rectum & Anus
Pancreas
General Histology of Digestive System
1. Mucosa
Lined by epithelium
Loose connective tissue
Lamina propria (BV, LV, glands, Peyer’s Patches (Ileum))
Muscularis mucosae (IC/OL SMC layer)
2. Submucosa
Surrounded by dense irregular (fibroelastic) connective tissue
Glands, BV, LV
Parasympathetic nerve tissue (Meissner’s submucosal plexus)
3. Muscularis Externa
IC/OL SMC layer
Parasympathetic nerve tissue (Auerbach’s myenteric plexus)
4. Serosa/Adventitia
May be surrounded by simple squamous epithelium of visceral peritoneum
Esophagus
1. Mucosa
Epithelium | stratified squamous non-keratinized epithelium
Cellular component | Langerhans cells (macrophages, APC)
Lamina Propria | esophageal cardiac glands (compound tubular)
Muscularis Mucosae | single layer of longitudinal SMC
2. Submucosa
Connective Tissue | dense irregular fibroelastic connective tissue
Key ID | esophageal glands proper (compound) – mucous cells & serous cells
3. Muscularis Externa
Upper third – skeletal muscle
Mid third – skeletal and smooth muscle
Lower third – smooth muscle
Stomach
1. Mucosa
Epithelium | simple columnar epithelium
Cellular component | surface lining cells, parietal cells, regenerative cells, mucous neck cells, chief cells, enteroendocrine cells, NO goblet cells
Lamina Propria | loose connective tissue, gastric glands (simple tubular)
Muscularis Mucosae | IC/OL SMC layer & third circular SMC layer
2. Submucosa
Connective Tissue | dense irregular collagenous connective tissue
3. Muscularis Externa
Inner oblique SMC
Middle circular SMC
OL SMC

Pyloric Stomach

Fundic Stomach

Cardiac Stomach

Stomach Cross Section
Small Intestine Common Features
1. Mucosa
Valves of Kerckring/plicae circulares
Villi | differs between the regions
Epithelium | simple columnar epithelium, Crypts of Lieberkhun (simple tubular or branched tubular glands)
Cellular component | surface absorptive cells (brush border), goblet cells, enteroendocrine cells, regenerative cells, EED cells, Paneth cells
Lamina Propria | reticular tissue, BV, LV, SMC
Muscularis Mucosae | IC/OL SMC layer
2. Submucosa
Valves of Kerckring/plicae circulares
Connective Tissue | dense irregular fibroelastic connective tissue
3. Muscularis Externa
Connective Tissue | thin layer of fibrous connective tissue
Nerve Plexi
IC/OL SMC layer

Duodenum

Jejunum

Ileum
Small Intestine Differing Features
Duodenum
1. Mucosa
Villi | leaf shape
Cellular component | goblet cells
2. Submucosa
Key ID | Brunner’s glands (compound tubular/branched)
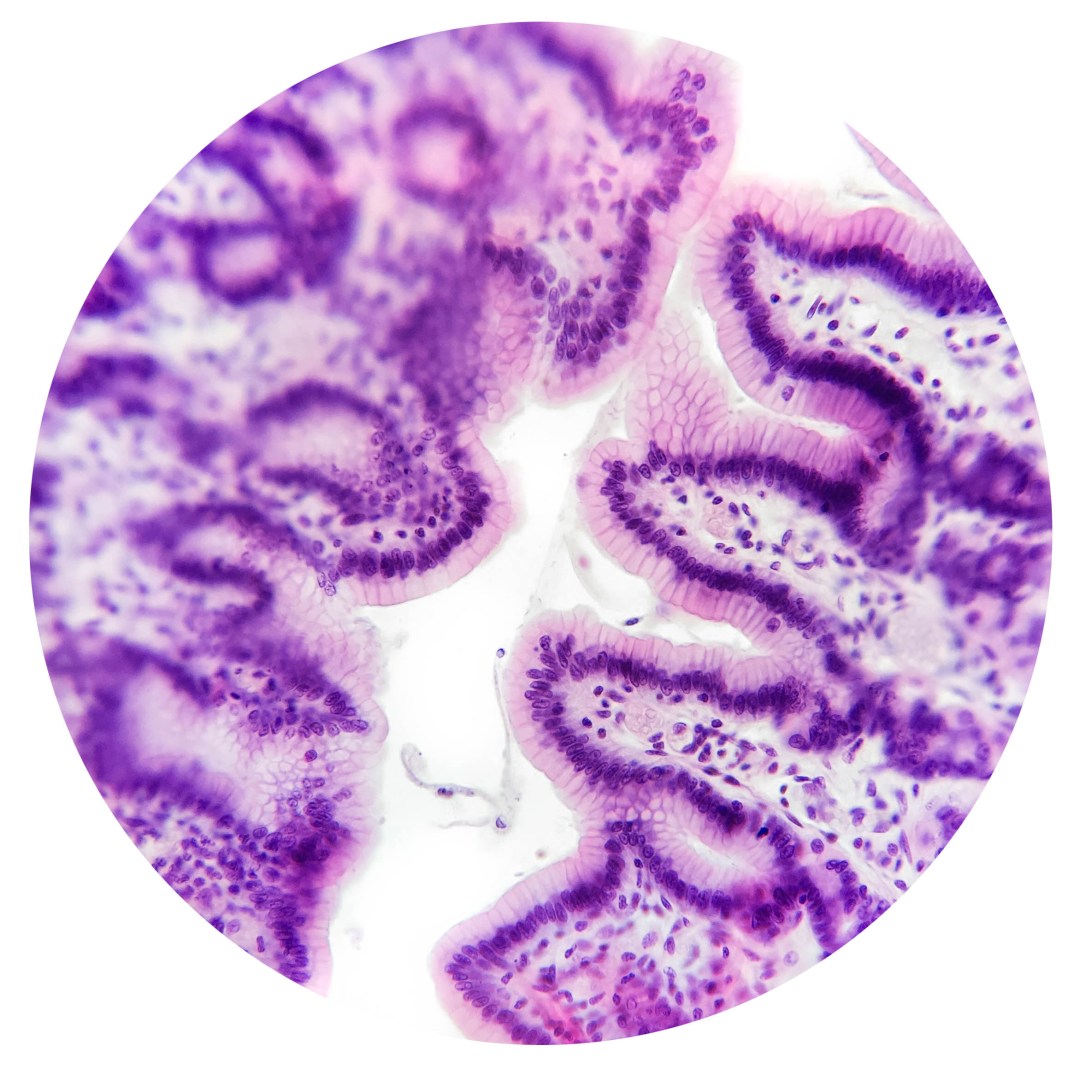
Jejunum
1. Mucosa
Villi | finger-like
Cellular component | more goblet cells
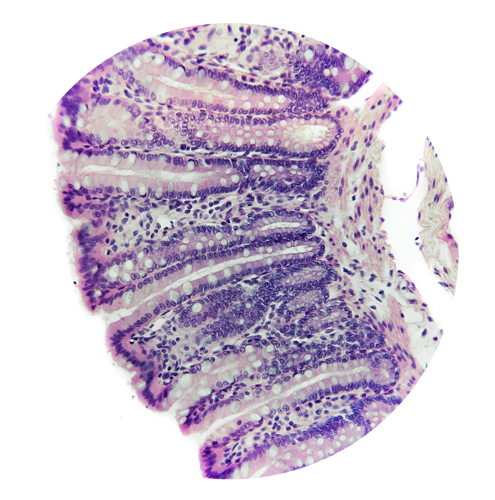
Ileum
1. Mucosa
Villi | club-like
Cellular component | even more goblet cells
Lamina Propria | Peyer’s Patches
2. Submucosa
Key ID |more lymphoid tissue
Large Intestine
Colon
1. Mucosa
NO Valves of Kerckring/plicae circulares
Villi | NO villi
Epithelium | simple columnar epithelium, crypts of Lieberkhun
Cellular component | lots of goblet cells, absorptive cells, NO Paneth cells
Lamina Propria | more lymphatic tissue (lymph nodules), long simple tubular glands
Muscularis Mucosae | IC/OL SMC layer
2. Submucosa
Lymphatic tissue
3. Muscularis Externa
Teniae coli
Nerve Plexi
4. Serosa
Adipose tissue

Colon

Appendix
Appendix
Structure closely resembles that of the colon
1. Mucosa
NO Valves of Kerckring/plicae circulares
Villi | NO villi
Epithelium | simple columnar epithelium, crypts of Lieberkhun
Cellular component | lots of goblet cells, absorptive cells, NO Paneth cells
Lamina Propria | more lymphatic tissue (lymph nodules), long simple tubular glands
Muscularis Mucosae | IC/OL SMC layer reduced
2. Submucosa
Lymphatic tissue extending to submucosa
3. Muscularis Externa
Teniae coli
Nerve Plexi
4. Serosa
Adipose tissue
Rectum & Anus
Resembles colon except:
Mucosa in the Anal Canal transitions from simple columnar epithelium to stratified squamous non-keratinized epithelium to stratified squamous keratinized epithelium at the anus
Increase in goblet cells, adipose tissue, and thicker teniae coli
Pancreas
Exocrine
Stroma | thin dense irregular connective tissue
Parenchyma | acinar cells
Glands | compound tubuloacinar gland
Duct system | centroacinar cells, simple columnar cells, goblet cells, EED cells
Endocrine
Islets of Langerhans | alpha cells (glucagon), beta cells (insulin), D cells (somatostatin), G cells, PP cells